
Ulrike Wohlleben
Eating and Communicating as Intertwined Activities
Preliminary remarks:
“Say, let’s go out for a beer again sometime!”
What exactly is the content of this proposal?
Is it primarily about the beer, or the associated opportunity to have a good talk, and to at last get caught up with one another again?
Eating and drinking are life-affirming activities. They offer us sustenance, enjoyment, relaxation and an occasion for conversation, laughter and celebration. As life-affirming activities, eating and drinking are naturally best when shared with others.
Eating and communication are thus closely connected to one another in our daily lives. Emotional and social circumstances can turn eating and drinking into memorable experiences of well-being (“Grandma’s apple pie is still the best!”) or regret (“Even the coffee they served before the interview was lukewarm!”).
What questions do Castillo Morales® therapists seek to answer?
Given the concept’s aim of enhancing the capacity of individuals to participate in daily activities and its emphasis on opening channels of communication as a means to doing so, it is self-evident that eating and drinking also play a central role in
Castillo Morales® therapy. With a developed sense of appreciation and curiosity, we Castillo Morales® therapists regard ourselves as “co-diners” – as persons who first attempt to identify and participate in the uncomplicated and successful means of eating and drinking the family and the child have already discovered. Using this as a basis, we then work carefully together with them to find ways of bringing about desired improvements.
We approach the therapeutic support we offer to people who need assistance with eating and drinking by seeking to answer two questions:
- How do adults and children eat together with their families if they are not able to manage this important aspect of their everyday lives on their own?
- What form of assistance can we as Castillo Morales® therapists offer to such adults and children and their families?
What resources do Castillo Morales® therapists make use of?
We assume the validity of the following three hypotheses:
- Eating and drinking with others presents an opportunity for fun and enjoyment.
We begin by observing what already works well for our clients. What are the preferred foods and beverages? When, where and with whom do our clients like to eat best?
While observing we try to find out whether existing preferences are based on taste, convenience or both taste and convenience. We also try to determine the degree to which hunger plays a role and whether giving more attention is experienced as helpful or disturbing. - Eating and drinking take time and appropriate means.
We record the variables that have so far enabled a child or an adult to eat and drink. Noteworthy details include: table positions; times of day; effective implements (e.g. bottles and utensils);and effective forms of assistance performed by those affected and their family members. - Eating and drinking require adequate functional processes.
Using our expertise, we can now evaluate the functional activities of sucking, swallowing and chewing in connection with the position of the body (sitting or lying) and the visual and taste-oriented opportunities to recognize the food that is served. Depending on the primary diseases involved, it will be necessary to draw distinctions among the following difficulties:
Primary Diseases That Can Lead to Limitations in Eating and Drinking
There are many different conditions that make it difficult for very many people to eat and drink. These many different conditions cannot all be meaningfully and tidily subsumed under the term dysphagia (impaired ability to swallow). In what follows, we describe some of the most common conditions that affect infants and small children. We will address such limitations with reference to adult patients in a separate context.
- Sucking impairment
While many children with hypotonia (low muscle tone), rapid muscle fatigue and certain cardiovascular diseases are able to suck, swallow and chew adequately, they tend to reach a point of fatigue rather quickly. This is why they stop drinking or eating after a few swallows or bites and, exhausted, fall asleep before reaching the point of satiation. This will prevent them from gaining weight and flourishing. - Dysphagia
Dysphagia is diagnosed for many different disorders that affect the process of swallowing. For various reasons, any or all of the stages of the swallowing process may be disrupted or become disrupted in infants, children and adults. An attempt to list all of the reasons would go beyond the scope of the present discussion. In addition to our clinical observations of symptoms such as coughing, choking, wet voice, and persisting fever of unknown origin(to name a few),it is essential in such cases for the patient to undergo diagnostic imaging at an early stage in order to avoid serious risks associated with choking and pulmonary aspiration while eating and drinking. Many hospitals and clinics offer special imaging procedures and clinical examinations that enable therapists and physicians to arrive at precise diagnoses. - Organic-functional changes involving orofacial or gastrointestinal systems
Infants and children with the following conditions may be affected by such changes:
- Genetic disorders
- Infantile cerebral palsy of various classifications and manifestations
- Premature birth or small for gestational age (SGA)
- Congenital defects or traumatic injuries to the face, mouth, trachea or esophagus
What are some of the main concerns of the parents?
The relationship of a mother to her newborn can be fundamentally influenced by her capacity to feed the newborn. The image of a hungry infant who promptly empties its mother’s breast or a bottle with powerful sucking action and then peacefully falls asleep after a brief and jolly round of burping reflects a deep-seated wish on the part of many mothers for recognition of their maternal competence.
It can be especially confusing and deeply troubling when this cherished aspect of motherhood is disrupted during the very first hours, days or weeks of a child’s life.
“Our main issue from the very beginning was feeding. It dominated our lives from the beginning. We experienced ups and downs, were often frustrated, annoyed, discouraged, and exasperated. Essentially, we were obsessed by the process of feeding and tube feeding. We sometimes had the feeling it would never end.”
(Excerpt from a report written by the mother of a boy with CHARGE syndrome, summer 2013)
“It was difficult at the beginning to be patient while feeding, to stay calm, to continue to offer milk no matter what . . . At first I chastised myself for looking on so long in January, and now M. wasn’t able to grow and flourish on account of me.”
(Excerpt from a report written by the mother of a girl with a respiratory chain disorder, spring 2013).
While the statements made by the parents vary depending on the specific disabilities of their children, there are clearly a number of basic concerns they share.
Parents worry in the following situations:
- Eating and drinking involve a tremendous and worrisome degree of physical effort. Suffering predominantly from movement disorders, the children have a difficult time mastering the complex actions of sucking, swallowing and chewing. For our part, we admire the parents and their children for their perseverance, resourcefulness and patience as they pursue their goal of being able to enjoy delicious and sustaining meals together. One big advantage here is that children generally like to eat and their hunger provides plenty of motivation.
- Their children do not eat and drink enough to gain weight and develop in the desired manner. This relates primarily to infants and babies who were born premature or small for gestational age (SGA). Their mothers tend to be perplexed by the minimal amounts of food and drink their children consume, and they feel stressed by the continuous effort to get their children to eat and drink “at least a little bit more.”
- Their children spit up too much and therefore fail to gain weight. We frequently observe this in children with certain cardiovascular diseases. Long-term tube feeding can also lead to vomiting, for instance, whenever children don’t tolerate the formula as well as expected on account of its composition or the amounts prescribed by the doctor.
- Their children turn out to be picky eaters, accepting only a small variety of foods, flavors and consistencies. We observe this frequently in children with hypersensitive mouths. These children may struggle to the point of aversion and regurgitation with the perception, processing and breaking down of solid foods. From the perspective of the child, there may even be emotional reasons that speak against varying the types of food and beverages that are served (in another context this is referred to as feeding disorders).
What does the Castillo Morales® concept offer?
We develop our support regimens on the basis of the above-mentioned three hypotheses. Working closely together with our clients, we identify appropriate activities enable and promote an enhanced degree of participation.
Goal 1: Sharing fun and pleasure with others
Meals at the family table that include the use of suitable chairs and utensils are primarily an opportunity to come together to talk and enjoy food and beverages.
We recommend regarding eating and drinking as an important part of family life:

- Eat meals together as often as possible.
- As parents, take account of your own appetite and nutritional needs.
- Converse with one another instead of focusing in a worried manner exclusively on the amounts consumed.
- Make a conscious effort to create a stimulating environment. Do not focus only on child-appropriate utensils. Consider other things such as flowers on the table, humorous utensils or the test use of utensils that are otherwise reserved only for the adults, for instance, allowing children to drink water from papa’s beer glass or to take a sip of mama’s cappuccino.
- Give children a view of a larger segment of the whole process. Go grocery shopping together, distribute the food to the appropriate locations in the kitchen and cook in the presence of and with the assistance of the child. Consider the tactile and gustatory sensations associated with food. Prepare food with care and in a manner suitable for children.
Goal 2: Taking the time to learn and discover new things
We regard the often time-consuming situations in which children and adults need to be fed as far more than lost time. On the contrary, these situations present opportunities for training and learning. After all, many of the forms of functional support in the narrow sense of the word – see below – also support the activities of eating and drinking. There is no need to take extra time for training. Indeed, eating and drinking can also be used to learn functional processes in a pleasant context (upright sitting positions, guiding a hand or utensil to one’s mouth, opening and closing ones mouth, lateral tongue movements, etc.).
Getting used to new consistencies and flavors presupposes a variety of dishes on a number of consecutive days. Changing the available variety of foods too frequently, however, will not allow the children to take a step-by-step approach to becoming acquainted with new things.
Goal 3: Working out the most adequate functional processes for daily use
This is an area in which Castillo Morales® therapists profit from their extensive repertoire.
- The therapists can help to ensure that the children experience their food with all of their senses, i.e. the sense of sight, smell, taste and touch.
The result is that the mother helps her child to assume an advantageous posture and to eat as independently as possible. With her bended left leg and her left arm, she can provide the necessary stability, present the food in a manner that engages the senses and use this as a subject of conversation.

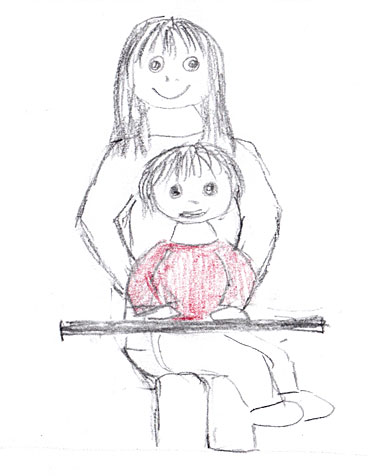
- The therapists can help to ensure the proper position of the child on her mother’s lap so that the child’s head remains as stable as possible and the child is better able to learn how to swallow. Paying attention to the rotation of the shoulder girdle in relation to the waist helps somewhat older children to use lateral lower jaw and tongue movements for chewing. The properly planted feet offer support and facilitate the swallowing process just as a properly positioned (upright) torso and neck. This too is supported by rotation.
The therapists can activate the muscles in the whole body, engaging the diagonal muscle chains as a means of facilitating orofacial functions such as sucking, swallowing and chewing. This essentially involves modeling the entire body, especially the torso, but also the feet and hands, which have an important sensorimotor connection to the mouth.

This child with hypertonia (e.g. in connection with bilateral spastic cerebral palsy) receives help from her mother who sits next to her so that she can support her child’s back, remain in contact with her and help to feed her. However, the girl’s legs are overextended and her feet are not well planted, preventing her from assuming a more properly aligned and stable sitting position and thereby having a greater degree of control over the movements of her head. While swallowing is possible in this position, it is more difficult.

Participation is also possible in the illustrated position. The child’s head may rest on one of its arms. The child’s torso remains supported by the table when food is spoon fed, when small bites are presented from the side and when the child prefers to take a break from feeding..

This child with hypotonia profits from the tilted seat, which distributes more weight to the feet, and the well-adjusted height of the table. The arrangement enables the child to sit upright on its own for a sufficient amount of time to enjoy eating.
Both positions were worked out together with the clients: the modeling of the feet, legs and torso, special exercises that help children to assume more favorable sitting positions on their own, and the selection of suitable aids or simple furniture solutions enable more activity and thereby improve participation, both at the dinner table and in children’s groups.
- The therapists can support parents when it comes to selecting special aids and accessories from among a broad range of products available on the market, products that are not all necessarily suitable. The important thing is that children are neither required to expend too much energy while sucking nor do they run the risk of becoming bloated because the milk flows too swiftly into their mouths. Soft spoons that can remain in the mouth for a short time when soft food is to be swallowed are helpful because they can facilitate proper tongue positioning and lip closing.
- The therapists can implement special measures from the Castillo Morales® concept to facilitate important functions such as sucking, swallowing(via basic exercises), chewing (via Variation I basic exercises),lip and cheek vibration) to gradually enable mother and child to achieve an easier, unburdened way of feeding, eating and drinking. In addition to weight gain, the aim is primarily to increase the acceptance and the satisfaction mother and child experience in their intimate, learning and sharing relationship with one another. The joy of being able to share meals together plays a central role in the concept because it is connected to both the gradual overcoming of functional or anatomic difficulties in daily activities and the positive development of the emotional and social conditions for enhanced participation in family life. In the words of Rodolfo Castillo Morales:
“Alimentar un nino es compartir la vida.”
“Feeding a child is sharing life.”
(Excerpt from an instructional manual)
Author: Ulrike Wohlleben
Speech Therapist and Clinical Linguist
Educational Therapist for the Castillo Morales® Concept